A new pre-print study from Norway looking at differences in outcomes between vaccinated and unvaccinated hospital patients has found that being vaccinated makes zero difference to the risk of dying once hospitalised for COVID-19.
“There was no difference in the adjusted odds of in-hospital death between vaccinated and unvaccinated patients in any age group,” the researchers write. They also observed no difference between vaccinated and unvaccinated in the length of hospital stay for patients not admitted to ICU. These findings are adjusted for age and other risk factors so are not simply due to the vaccinated being older or at higher risk (though, as always, the validity of the adjustments may be questioned). The findings also only include patients admitted primarily due to Covid, so aren’t confounded by patients admitted for other reasons who also tested positive at some point.
The researchers did however find that vaccinated patients aged 18-79 had “43% lower odds of ICU admission” and an estimated 26% shorter hospital stay than unvaccinated patients.
It is curious that vaccinated patients were 43% less likely to need ICU but no less likely to die. Did the antibodies from the vaccines just mean that those who were going to fight it off did so a bit more quickly and easily, but the vaccine antibodies weren’t actually able to save anyone who wasn’t going to survive anyway? That appears to be the researchers’ conclusion:
Our results suggest that once hospitalised the risk of death among vaccinated and unvaccinated patients in Norway is similar. However, for survivors the disease trajectory is milder in vaccinated patients, with reduced need for hospital care and organ support.
The study didn’t examine what difference vaccination might make to the risk of being admitted to hospital in the first place, as it was a hospital-based study. This means vaccination may reduce one’s risk of needing to go to hospital (and thus the overall risk of death), even if it doesn’t reduce the risk of dying once admitted.
The study covered all patients in Norway admitted to hospital primarily due to Covid between February 1st and September 30th 2021, though made various exclusions (including 154 who tested positive within 21 days of their first dose, which is a shame as more analysis needs to be done on such cases). It included 2,361 patients, 70 of whom (3%) were partially vaccinated and 183 (8%) of whom were fully vaccinated. Almost all had the Pfizer vaccine. Over the study period, 421 of the patients (18%) had been admitted to ICU. At the end of the study period 18 patients (0.8%) were still in hospital, while of the 2,343 patients discharged, 107 died in hospital (4.6%).
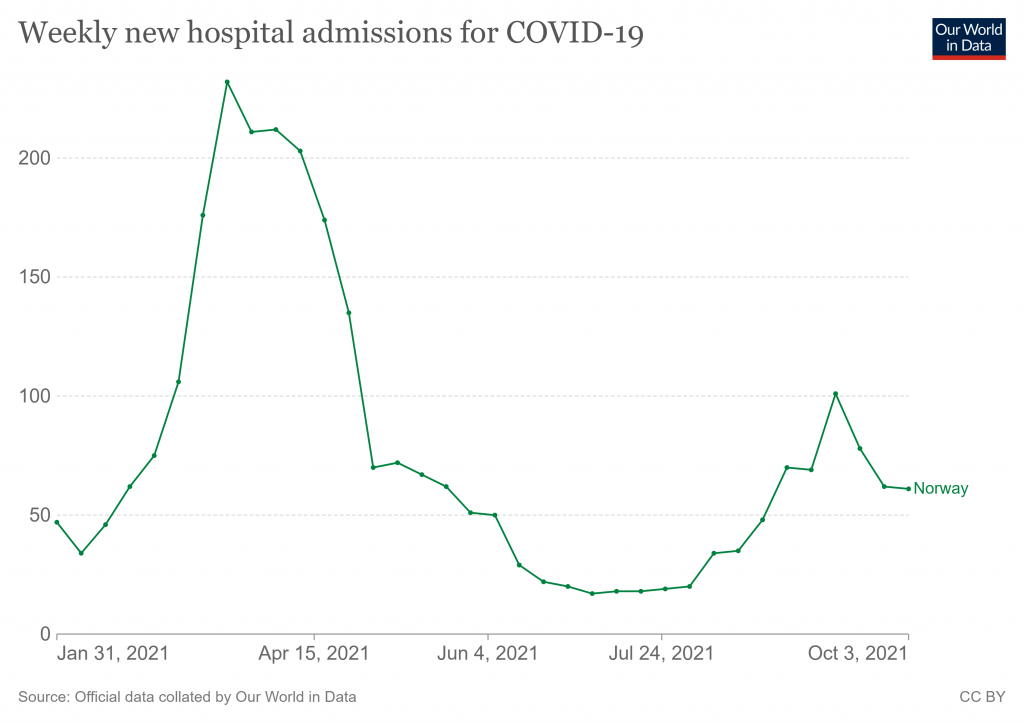
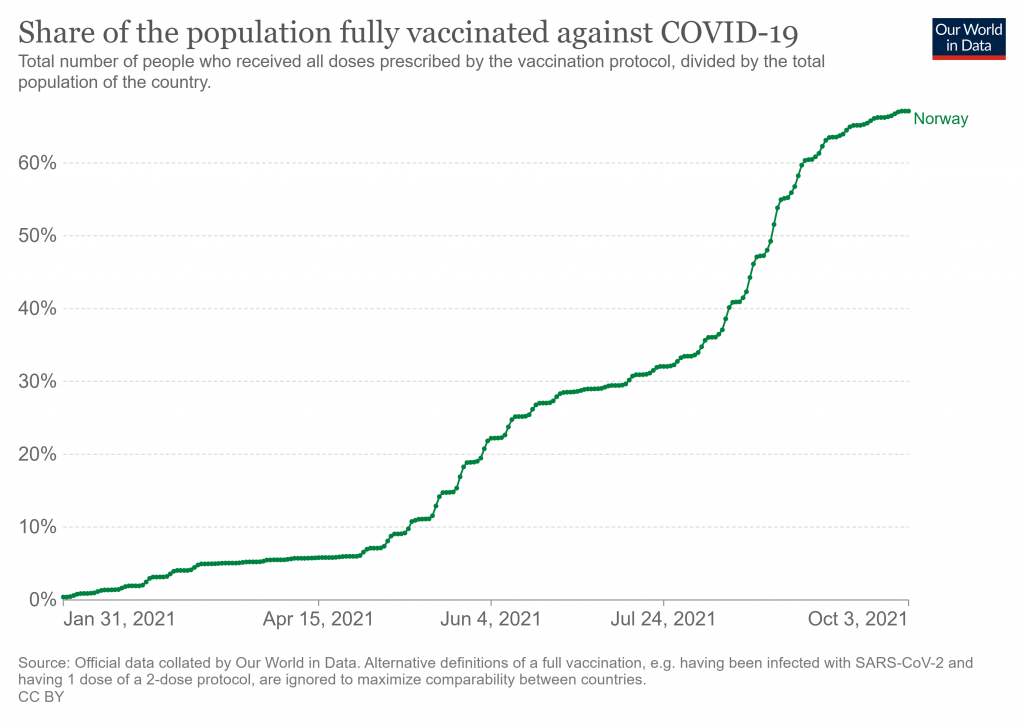
The percentage vaccinated seems at first glance to be very low at 8%, particularly as the study states that 84% of Norwegian adults were double vaccinated by the end of September. However, the figure makes more sense when you look at when Covid hospital admissions in Norway occurred during the study period: of the 2,775 total Covid hospital admissions during the period, 1,742 (63%) occurred before May 2nd, at which point just 7% of Norwegian adults were vaccinated.
In fact, the study tells us when people were admitted by vaccination status, as per the following table.
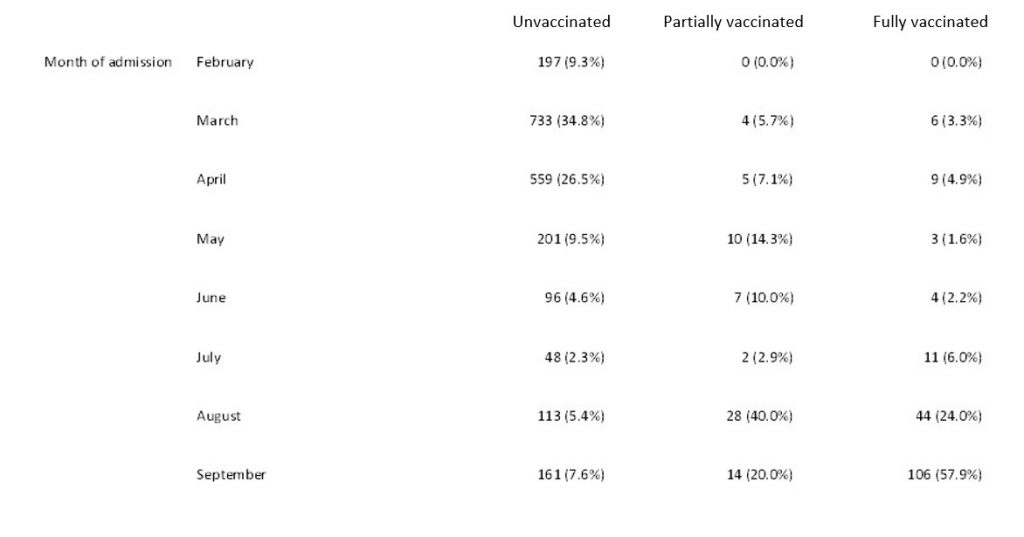
Note that 58% of the double vaccinated were admitted just in September, and 82% once you add August in as well, leaving only 18% admitted prior to the Delta surge. Is there a waning effect at work, then? Perhaps, though the authors don’t suggest so. In fact, they decline to include a chart showing how the risk of in-hospital death changed over time, explaining: “Date of admission was not associated with death in hospital in our multivariable model.” This suggests the trend was flat, rather than declining.
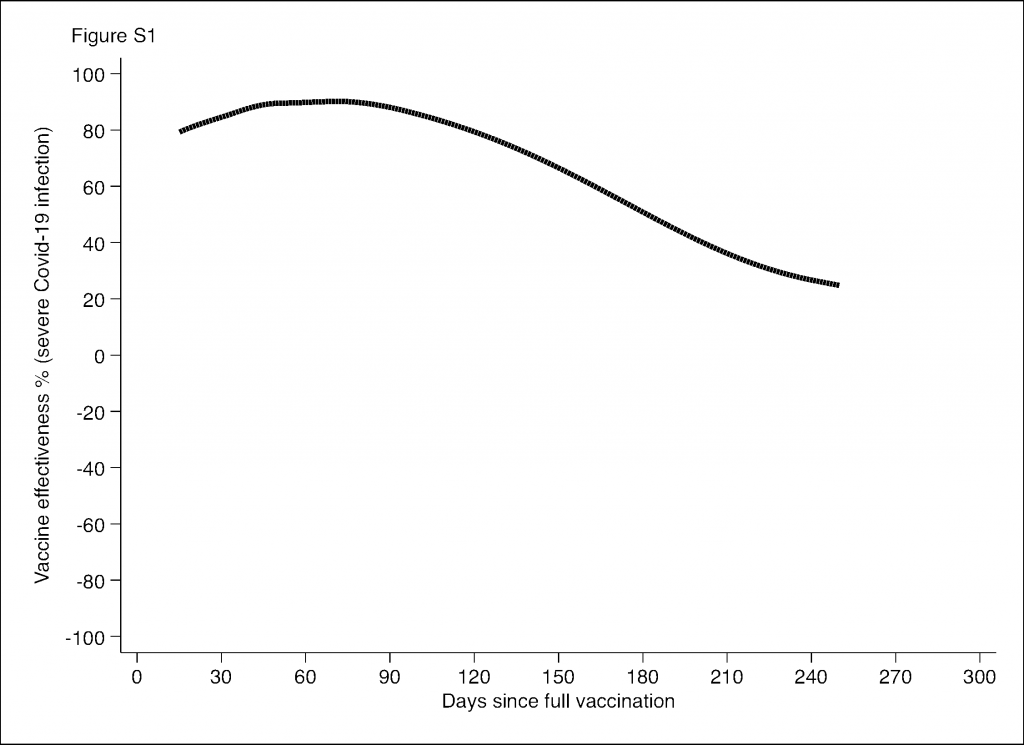
The study is unusual in finding zero vaccine effectiveness against in-hospital death for the whole period of the vaccination programme. A recent study in neighbouring Sweden found vaccine effectiveness against severe disease declining over the course of seven months to be low, zero or even negative in risk groups such as men, older frail people and people with comorbidities (see below; there were no separate findings on death). But this is one of the first major studies to find an important measure of vaccine effectiveness – in-hospital mortality – to be negligible overall.
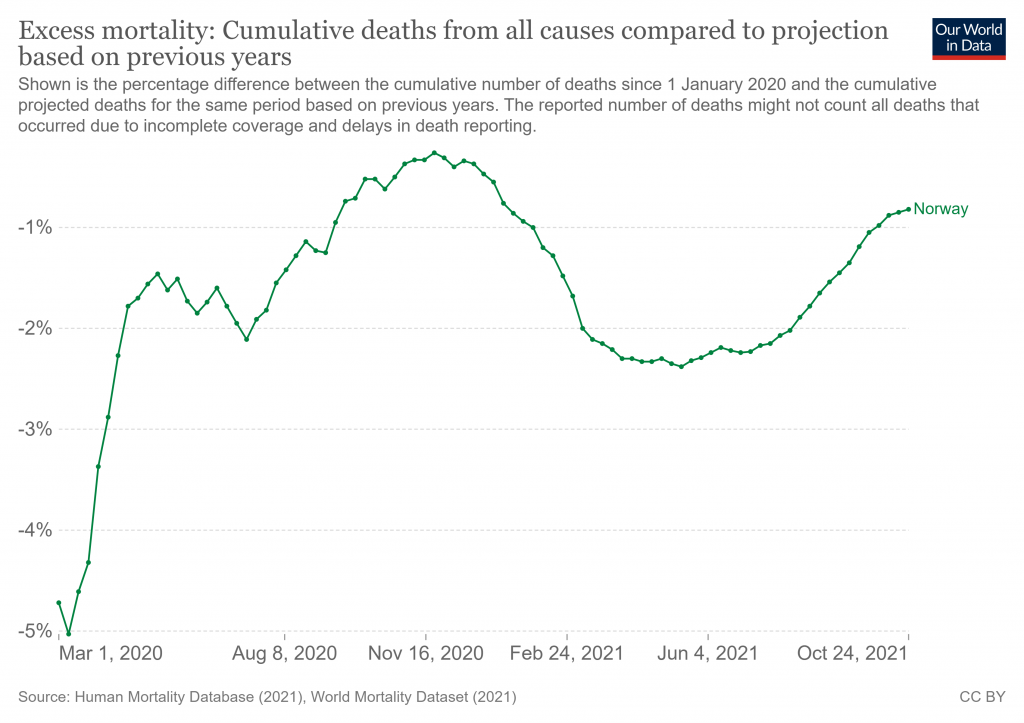
It’s probably worth recalling at this point that Norway is an outlier generally in the pandemic so far, with one of Europe’s lowest Covid death rates and, incredibly, zero excess mortality during the pandemic.
Does this affect how generalisable the results of the study are to other countries?
Similarly, Sweden is also unusual in having been left largely unscathed so far by the Delta variant that has caused new surges in most countries.
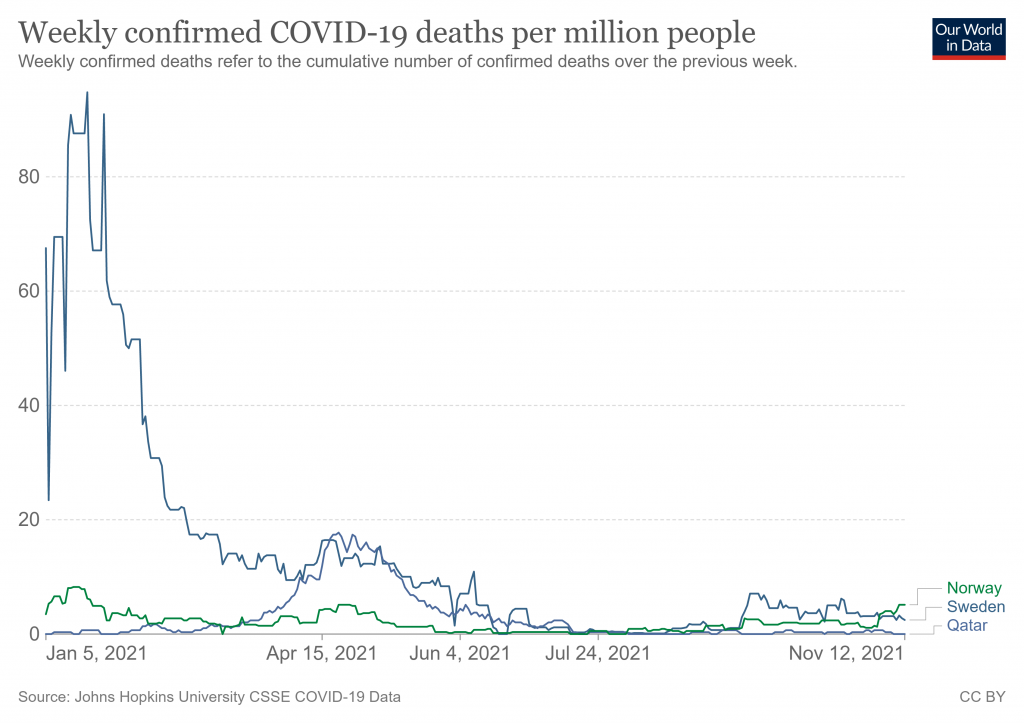
Qatar, too – another country where a recent study has found sharply declining vaccine effectiveness against infection – has seen very little impact from Covid in 2021. In this case the study found effectiveness against serious disease generally held up, though less so among those over 60.
Is there some connection between this low impact of Covid in 2021 in these countries and the vaccine effectiveness results showing declining or zero efficacy against serious disease and death? Something worth looking into, I’d suggest.
Article: Norway Study Finds ZERO Vaccine Effectiveness Against Death for Covid Hospital Patients